Level Up: Trending, Analyzing and Implementing Heart Rate Variability
Ep. 5 HRV & Stress Tolerance with Dr. Jay T. Wiles
By: Ariel Kamen, BSN RN
Biostrap is the most clinically validated wearable device to record biometric trends and is only the focal point of applied psychophysiology. This article synthesizes both episodes 5 and 51 with Know Your Physios’ HRV and biofeedback expert, Dr. Jay T Wiles. From Dr. Wiles, we learn about the gold standard biometric that top fitness trackers are able to calculate – heart rate variability (HRV). Stressors today have far exceeded our human threshold of stress tolerance. Learning the motives of HRV can stabilize our stress curve, achieve a state of ease in all levels of performance, and enhance our data-driven decision making.
What is HRV? 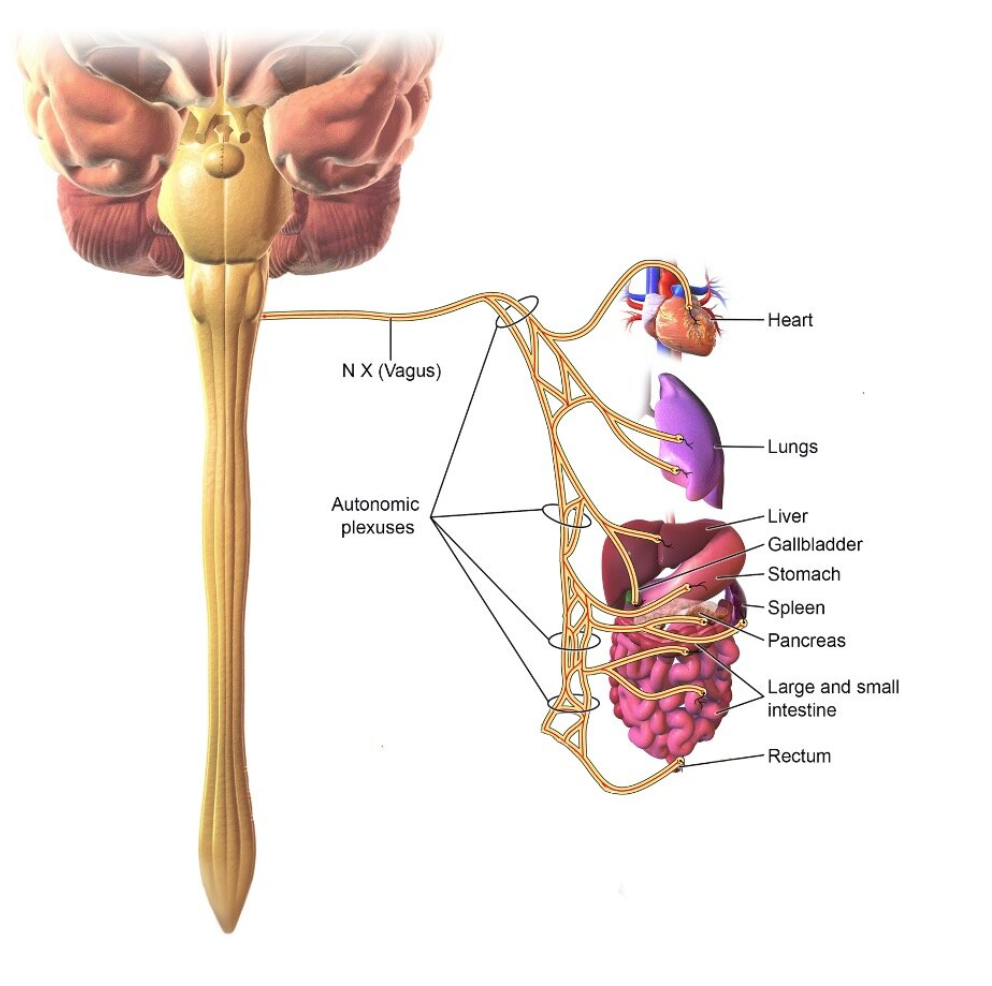
Heart Rate Variability is a sensitive biometric based on the subjective ability of the heart to change its rate depending upon the situation. As we would naturally expect, talking increases the heart rate, while meditation decreases the heart rate. Fluctuations between the heart rate and stress levels are occurring constantly throughout the day and night. Using RMSSD software, the Biostrap quantizes these fluctuations and represents it as HRV in milliseconds.
HRV reflects the integrity of vagus nerve-mediated autonomic control of the heart (Capilupi, Kerath & Becker, 2020). The vagus nerve is the 10th cranial nerve in the brain that innervates the heart and lungs in order to control HR, BP, and RR without our voluntary control. HRV analysis is linked with an understanding of the body’s interaction with environmental stress (Zhu, Ji & Liu, 2019).
Naturally the nervous system experiences fluctuations between sympathetic and parasympathetic responses depending on the given scenario. Living in chronic states of either nervous pathway poses risks for cognition and physical injury. 80% of vagal tone is afferent neurons (Bonaz, Sinniger & Pellissier, 2016) that transmit impulse towards the visceral organs from the brain and spinal cord.
In particular, the vagus nerve provides parasympathetic innervation to the gastrointestinal tract. Physiological roles of the afferent (sensory) and motor (efferent) vagus nerves provide profound regulation of appetite, mood, and the immune system. The pathophysiological outcomes of vagus nerve dysfunction may result in obesity, mood disorders, and inflammation (Browning, Verheijden & Boeckxstaens, 2017).
Physiology of HRV
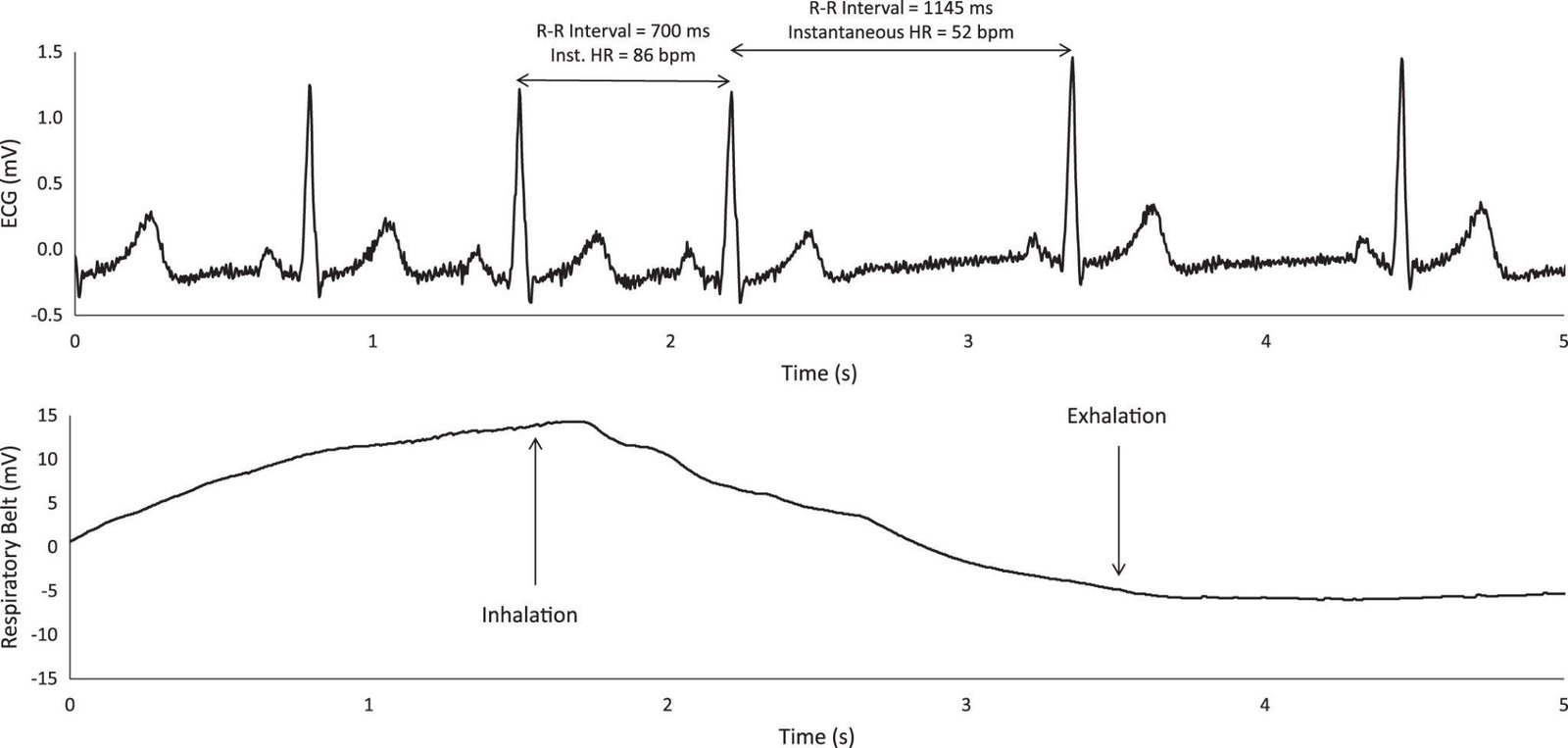
Heart rate variability (HRV) is a non-invasive method to evaluate heart rate (HR) regulation of the parasympathetic division of the autonomic nervous system (Kingsley & Figueroa 2016). Simply put, HRV refers to the beat-to-beat variance in the R-R interval during a given time period. The R wave is the electrical waveform for ventricular contraction, the “dub” that pumps blood to the brain and body. By looking at the waveform diagram below, we see one major contributor to HRV is the change in lung size during a ventilatory cycle: the R-R interval generally decreases during inhalation and increases during exhalation (Levin & Swoap, 2019). For high performance athletes, conscious incorporation of nasal breathing during training can have profound effects on HRV.
A study done by (Mol et.al., 2021) shows that higher HRV predicts greater chances of survival, especially in patients aged 70 years and older with COVID-19, independent of major prognostic factors; while lower HRV predicts ICU indication and admission in the first week after hospitalization. In general, health outcomes are related to the neuro-inflammatory responses that occur during the disease processes and how the body is able to accommodate fighting off the pathogen. Now more than ever, as our society transitions into endemic stages, we must strengthen our bodies. By trending our HRV using a wearable device, we can take the appropriate steps to adapt.
Physiology differs between the sexes. Emotion is said to be carried within musculature and serves as a guide for the autonomic nervous system. Dr. Wiles explains that men hold more muscular tension in their back and shoulders while women hold more stress in their scalp which appears as a headache. Sustained contraction of muscle tension tends to be high during emotional stress and states of high anxiety from (Goldstein, 1964). When the body thinks that it is under stress, it may create too much tension which may lead to decreased HRV and pain. Our mind and body are interconnected bidirectionally which allows us to consider our body and how it translates into our emotion and vice versa. 
The heart acts as a master pump for our body; transporting oxygen and nutrients afferently and accepting waste back efferently. When the body is in states of low heart rate demand and diminished blood flow, as seen during sleep and fasting states, HRV improves through activated parasympathetic responses. Simply stated, when food is not being digested, all of the blood that would have been used to break down nutrients is being focused to supply blood to the brain and heart.
Rhythmically, the heart is not a metronome. During increased activity, such as talking or inhalation, the heart rate increases. On the other hand, the heart rate decreases during moments of silence and exhalation. All together this phenomenon explains respiratory sinus arrhythmia (RSA): the natural fluctuation of heart rate in relation to breathing patterns. What we know is that when we slow breathing down, we increase RSA, and when we increase RSA it serves as the number one influencer to increase HRV. Innervations of the ANS ultimately shock the heart and cause it to beat variably. Key variables of HRV include sleep, fasting, muscle tension, and hydration. Demands of the heart decrease when the GI tract is empty and requires less blood flow. The more you KnowYourPhysio, you will be able to experience heart rate variablility through experiment with KYP’s actionable steps.
Remote Monitoring of HRV
HRV as a time domain index between heart beats, is a metric that biohackers use to quantify fluctuations in their vagal tone (i.e. autonomic nervous system) (Young & Benton, 2018). Most trackers are using RMSSD software as a measure of HRV, except the Apple Watch which uses SDNN (Dalmeida & Masala, 2021). Dr. Wiles encourages biohackers to use self-comparative analysis trends, meaning steer clear from comparing HRV within your community; because not only is HRV dependent on the device being used, but more dependent factors like genetics, BMI, diet, and inflammation are challenging to compare amongst users.
The Hawthorne Effect and How to Overcome It
Observation affects behavior as does trending scores. Wearable Devices provide continuous monitoring that can stimulate temptations to constantly check scores. Constant check of biometric data alters the data being collected. Subjects who are aware scored much higher than subjects who were unaware of their participation (De Amici et. al, 2020). According to Dr. Wiles, “when you have really good autonomic control, you can tell your nervous system exactly what you want it to do at will.” (Ep. 51 8:50-9:03).Fine tune training aligned with a health and wellness lifestyle is the force that overcomes The Hawthorne Effect.
So, where can we find clarity in autonomic control?
RPM is our high-fidelity snapshot of what’s going on, but to see where we are at, we really have to check in with ourselves. Dr. Wiles says, “It’s all good and well to have this biometric data, but data is secondary. Self reports use our qualitative feeling and subjective experience is actually our primary indicator of how we are doing.” (Ep. 51, 10:53) Dr. Wiles strongly discourages RPM users from immediately checking scores after waking from sleep. Constantly checking scores invites further phone usage and becomes counterproductive. Biometric awareness has the ability to influence how we really feel, for better or for worse. Subjectively checking in allows us to consider all things mental acuity, psychologically and physically. Asking ourselves, am I ready for today? Before checking Biostrap’s readiness score provides a more accurate assessment than the score alone.
Interoception is our ability to mindfully tap into our bodily functions. Things like respiratory depth and rate, blood pressure, muscle soreness and tension, and CO2 tolerance. What we are doing is leveraging technology to enhance our interoception by trending data that then allows us to notice patterns. Noticing what it feels like to be stressed in alignment with the biometric data offers us a full spectrum analysis of how ready we are for the day. Being authentic, honest, and candid with ourselves will prevent burnout by being able to identify when we are stressed and take action to ease the tension. Pushing through can be detrimental so we use RPM as a guide to quantize all our activity on the inside.
Self – Assessment
There exists a myth about HRV being high is good and low is bad, but Dr. Wiles says, “normal is good.” By this he means that living around baseline is most optimal for autonomic control. Baseline HRV is an individual and crucial metric of analysis. Baseline is typically a normative range between 5 – 10 milliseconds.
Knowing baseline HRV true to you will be the basis of your HRV self-assessment. HRV is wildly sensitive – having many confounding variables. Proper self-assessment can only be achieved by considering your normative range. Normative range differs for every user and provides an upper and lower range to base the analysis on. Contextually, cortisol and catecholamine release constantly fluctuates with time and thus alters heart rate variability throughout the day. Normative range allows us to consider what is going on if we drop too low or high outside of our baseline HRV.
After weeks of accumulating data, Biostrap provides users with baseline HRV. Sensors on the device capture high resolution measurements using photoplethysmography (PPG) deep within the skin – up to 10x deeper than green light to extract reliable biometrics.
Scores & Strategies
Gamification is the application of elements in the form of a game. Trending biometric data allows users to undergo a self-assessment which then allows them to adopt actionable steps as a way to ‘level up’ our HRV and over all autonomic function. It is paramount to understand that HRV scores are subjective in nature. Minimal benefits will arise from comparing HRV scores among colleagues and peers because HRV is only relevant in comparison to an individual’s baseline.
Classic symptoms of being below baseline include tired, foggy, stressed and lacking motivation. Classing symptoms of being above baseline include lower respiratory rate and muscle tension. Feeling light as a feather. When people are really engaged in a high HRV, mental acuity is enhanced. Once again, the feeling is more relevant than the score itself.
Anomalies of HRV scores are seen in individuals who are depressed. These users may see their HRV sky-rocket as an overcompensatory mechanism of the ANS to overcome burnout. When we identify the changes in our internal environment using biometrics, we also must consider whether these changes are reflective of practical physiology and our physical experience. There are infinite intervals to consider during HRV analysis, leaving Dr. Wiles hesitant to encourage us to check our scores throughout the day without any context.
Biohacking is designed to build and optimize our physiology in order to achieve states of high performance. By recording and analyzing biometrics, most notably, HRV, coupled with qualitative lifestyle modifications, we can gain a deeper insight into our past, present, and future states of health.
Actionable Steps to Improve HRV:
Dr. Jay T. Wiles says, “to improve HRV, step 1 is increasing your level of self-awareness.” Mouth breathers and chronically stressed individuals trend lower heart rate variability then those who practice slow through the nose. Breath work to achieve a respiratory rate between 6-8 breaths per minute causes physiological changes in CO2 tolerance. Once you determine baseline HRV score, see how exposing yourself to hypercapnic states through breath work alters your metrics.
- Buy a Biostrap to trend your HRV using code ANDRES10 https://shop.biostrap.com/
- Convert your breathing style to nasal breathing – refer to Ep. 30 for more about The Oxygen Advantage
- Practice slowing your breathing to <6.5 breaths per minute to increase your CO2 tolerance
- Mindful breathing before workout and sleep
- Effective sleep to regulate the ANS
- Dark room
- Quiet
- Warm
- Movement throughout the day to tire body
- Empty stomach
- Hydration
- Forms of eustress
- Cold Exposure
- HIIT
- Fasting
- Non-surgical vagal stimulation
- Yoga
- Tightening the perineal muscles
- Meditation
- Gargling water
- Singing, humming, and or laughing
Resources:
Bonaz, B., Sinniger, V., & Pellissier, S. (2016). Anti-inflammatory properties of the vagus nerve: potential therapeutic implications of vagus nerve stimulation. The Journal of physiology, 594(20), 5781–5790. https://doi.org/10.1113/JP271539
Browning, K. N., Verheijden, S., & Boeckxstaens, G. E. (2017). The Vagus Nerve in Appetite Regulation, Mood, and Intestinal Inflammation. Gastroenterology, 152(4), 730–744. https://doi.org/10.1053/j.gastro.2016.10.046
Cygankiewicz, I., & Zareba, W. (2013). Heart rate variability. Handbook of clinical neurology, 117, 379–393. https://doi.org/10.1016/B978-0-444-53491-0.00031-6
Capilupi, M. J., Kerath, S. M., & Becker, L. B. (2020). Vagus Nerve Stimulation and the Cardiovascular System. Cold Spring Harbor perspectives in medicine, 10(2), a034173. https://doi.org/10.1101/cshperspect.a034173
Dalmeida, K. M., & Masala, G. L. (2021). HRV Features as Viable Physiological Markers for Stress Detection Using Wearable Devices. Sensors (Basel, Switzerland), 21(8), 2873. https://doi.org/10.3390/s21082873
De Amici, D., Klersy, C., Ramajoli, F., Brustia, L., & Politi, P. (2000). Impact of the Hawthorne effect in a longitudinal clinical study: the case of anesthesia. Controlled clinical trials, 21(2), 103–114. https://doi.org/10.1016/s0197-2456(99)00054-9
Goldstein, I.B. (1964). Role of Muscle Tension in Personality Theory. Psychological bulletin, 61, 413–425. https://doi.org/10.1037/h0040472
Kingsley, J. D., & Figueroa, A. (2016). Acute and training effects of resistance exercise on heart rate variability. Clinical physiology and functional imaging, 36(3), 179–187. https://doi.org/10.1111/cpf.12223
Levin, C. J., & Swoap, S. J. (2019). The impact of deep breathing and alternate nostril breathing on heart rate variability: a human physiology laboratory. Advances in physiology education, 43(3), 270–276. https://doi.org/10.1152/advan.00019.2019
Mol, M., Strous, M., van Osch, F., Vogelaar, F. J., Barten, D. G., Farchi, M., Foudraine, N. A., & Gidron, Y. (2021). Heart-rate-variability (HRV), predicts outcomes in COVID-19. PloS one, 16(10), e0258841. https://doi.org/10.1371/journal.pone.0258841
Young, H. A., & Benton, D. (2018). Heart-rate variability: a biomarker to study the influence of nutrition on physiological and psychological health?. Behavioural pharmacology, 29(2 and 3-Spec Issue), 140–151. https://doi.org/10.1097/FBP.0000000000000383
Zhu, J., Ji, L., & Liu, C. (2019). Heart rate variability monitoring for emotion and disorders of emotion. Physiological measurement, 40(6), 064004. https://doi.org/10.1088/1361-6579/ab1887
Picture 1: Lichtenstein, B. (2020, May 24). What is HRV? The Breath Space. Retrieved March 1, 2022, from http://thebreathspace.com/journal/2020/5/24/what-is-hrv
Picture 2: Levin, C. J., & Swoap, S. J. (2019). The impact of deep breathing and alternate nostril breathing on heart rate variability: a human physiology laboratory. Advances in physiology education, 43(3), 270–276. https://doi.org/10.1152/advan.00019.2019