In this episode, we chat with Chuck Hazzard, who is the VP of Wearables and Integrations at Heads Up Health, founder of The Human Optimization Project, and former VP of Sales at Oura. He brings his vast experience to this conversation all about wearable technology, and the benefits, downsides, and ethics around this tool for health optimization. We also discuss the future implications of this tech and how to apply and interpret the best and latest innovations to optimize your health. This conversation also examines the current use of such devices for fitness professionals as well as the average person, and delves into the ways using yourself for study will impact your life – but not always for the better if there isn’t adequate knowledge around what the metrics actually mean. Finally, Chuck shares some interesting insights into nocturnal biometrics, how lasers really are the way of the future, and the favorite devices and tools that he uses in his own life! To join in this relevant and inspiring conversation, tune in today.
→ check out OURA here Accurate Health Information Accessible to Everyone
→ check out Heads Up Health
____________________________________________________________
The Future of Data Collection
by: Ariel Kamen, BSN, RN
How curious are you to KnowYourPhysio? Are you wondering how to quantify your health? Can the average person use biometric data? Where does biometric data come from? If you find yourself curious about any of these answers, consider yourself lucky, because Chuck Hazzard, a founding father of wearable devices, has dedicated his expertise to KnowYourPhysio using wearable technology.
Wearable technology is an umbrella term for a plethora of devices whose aim is to quantify health. Biostrap, Apple, and Oura Ring are only the tip of devices that measure biometric data. Functionally speaking, wearable technology uses light emitting diodes (LED) or laser technology to penetrate deep beneath the skin and calculate all things heart rate, sleep, and oxygenation. Wearable technology provides evidence based data that is unique to you – for you to implement an n=1 study on yourself.
Implementing different habits, strategies, lifestyles, and biohacks can only be improved upon using trend analysis (Rudin et. al, 2020). Without measurements, our lifestyle choices are intangible. Wearable technology, literally, provides measurements at our fingertips, to up our performance and enhance recovery solutions.
Shifts Towards Telehealth Amidst Pandemic
During the pandemic, society experienced thorough cultural shifts. Panic encapsulated hospital systems; as census increased of people with respiratory disease while overall census decreased because families avoided emergency rooms with fear of contracting the corona virus. Crazy enough, 11,570,561,613 vaccines have been administered (as of 6/16/2022). That is 11.5 billion humans agreeing to an injection in the name of health. Public health concerns give unforeseen momentum into all things telehealth and remote patient monitoring (RPM). Currently, the two biggest barriers to wearable technology are lack of FDA approval and limited insight into biometric data interpretation. Without FDA approval, licensed physicians are skeptical of the accuracy and reliability surrounding wearable technology; although in some cases, the integration of wearable devices are being used for early detection of COVID-19 (Wong et. al, 2020). We have reached a singularity where health does not require assessment at the bedside, rather can be done from home.
Information Overload
Many wearable devices dump data into apps without providing individualized interpretations of the data. As a new area of study, biometric data analysis has led many experts, including KnowYourPhysio’s wearable device expert, Chuck Hazzard, to connect device users with RPM coaches who are certified in data interpretation and personalized guidance based on biometric data.
Further foreshadowing into the world of wearable technology, companies like Span Health and Heads Up Health are using machine learning software to provide individualized reports that dive deeper than current generalized reports by Fitbit and Apple Watch. These advancements in wearable technology beg Andrés to question: Is it ethical to give people access to biometric data and will people make the best decisions using the data reports?
Unfortunately, average users with minimal physiologic background have no idea whether SpO2% is ‘good’ or ‘bad’, let alone the actual definition of the metric. Research shows that users appreciate knowledge of their activity, but the device itself did not serve as a motivator to change behavior (Centi et. al, 2019). At the core of high performance is the desire to improve. How can we expect improvement if we don’t know where we currently stand?
Companies that sell wearable devices are not necessarily in the market of guiding users why they should care or wear the device. Their pursuit is that of profit marginalization and getting the product onto user’s wrists. Markets are not requiring data-integrity; markets demand processing speed and functionality. Other concerns of RPM are related to pricing. How much should it cost? And would prices depend on pathology or group settings?
RPM in Health Care 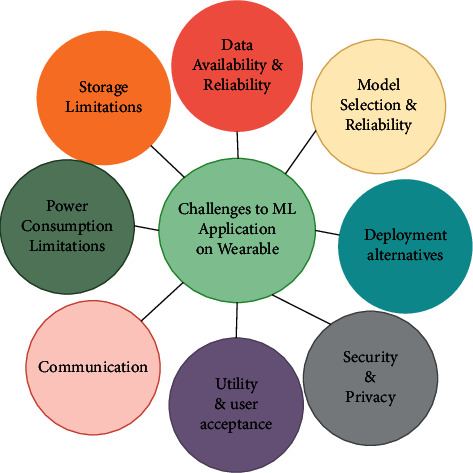
Remote patient monitoring (RPM) possesses potential in modern health care to allow for interpretation of health in between appointments. What happens with a patient’s physiology in between appointments can be monitored using wearable technology to quantify whether protocols are effective and parameters are being met.
Centers for Medicare and Medicaid Services (CMS) have reimbursement codes available for remote patient monitoring that cover initial set up costs and patient education. Thirty states have some form of reimbursement for RPM in their Medicaid programs. Validation studies can only be paid for by the device companies, providing further limitations to the legitimization and integration of wearable technology in health systems (Sabry et.al, 2022).
We know that wearable technology to self – quantify biometric data impacts decision making by the individual. The very knowledge of data influences the results of the procedure (Bryson, Arthur & Easton, 2021). Experts at KnowYourPhysio are trying to keep it simple, that is, serve as a catalyst to remove any barrier obstructing users from digging deeper into their health data.
Applications of RPM
Imagine tuning into a radio station each morning to hear about your nocturnal biometrics and readiness scores for the day. As of today, scores are flawed because they generalized, but advancements in wearable technology are addressing these flaws. Who is to say these scores even matter? How can the average person interpret and make decisions surrounding biometric data without the day to day use of health coaches? Is the average person able to dismiss a ‘bad score’ in order to perform? Functional Medicine movements are bridging the gap between behavioral science and health communications to integrate beneficial lifestyles with users.
As advancements in wearable technology continue to improve, clinical trials by Rockley photonics (funded by Apple) are using lasers to pull richer data from devices that are good enough to trend (Kent, 2021). Current metrics for instance, HRV, respiratory rate, and oxygen saturation provide a narrow view into physiologic functioning, which could be broadened with measurements of blood pressure and glucose shifts. Health care costs are dominated by metabolically broken people with hypertension and obesity (Chapel et. al, 2017). Advancements in wearable technology will one day serve as early detection of metabolic dysfunction and afford intervention before the scale tips past the point of incomprehensible costs.
Sleep Scores
Nocturnal biometrics measure biometric data while the user is asleep. Interestingly enough, the best time to monitor blood pressure is while asleep (Hermida et. al, 2014). Holistic health approaches are limited by lack of data during sleep. Blood pressure significantly fluctuates depending on the time of day, due to the dawn effect of cortisol oscillations and daily stressors, rather than heart rate which is best analyzed and averaged over 24 hours. Heart rate variability, for example, is almost meaningless throughout the day due to minimal autonomic restoration during wakefull states.
Averaging what happens during the night is perfect because the body is not exposed to external things – there are no confounding variables to influence what is going on. One day, we may see embedded devices used to collect biometric data behind the scenes of the user’s day to day life. As we transition into a ‘Smart’ world, the entirety of our lifestyle could cater to our physiological needs for us to stay optimized. One day, everything we touch and look at will monitor us in a positive way and be able to adjust our meal times and meeting schedules to best align with our peak physiological function.
Technological Takeover
Applied scientist, John von Neumann, started the conversation about a hypothetical point in time called the technological singularity – when advancements in technology surpass human intelligence beyond return (Colombetti, 2014).. We may one day see the rate of aging change when a person leaves their ‘smart’ apartment filled with hypoxia tents and lamps to simulate altitude and light, even if people thousands of years ago did not have these advancements.
While Web 3 development is underway, our brains are simultaneously humming along to the magical symphony of circadian rhythm. Our brains interpret and implement a lifestyle based on data from the day (i.e. air temp, overcast, time). Think about it, in the winter when air temps are cooler, we modify our behavior by wearing a jacket. This same principle can be applied to wearable devices and biometric data. HRV may symbolize the air temperature – are the skies windy or warm and still? What can we accomplish in these given conditions?
Open and honest engagement with biometric data guides our most basic behaviors.
Reasons to Wear a Device
Wearable devices and biohacking technology are expensive ways to mimic nature, although costs can be alleviated using free energy from the sun, or natural stimulation by nasal inhalation. High achieving individuals yearn for consistency and discipline, but taking ‘holidays’ from wearable technology allows the body to recenter without data-influence. Our host, Andrés Preschel, mentions the importance of taking the devices off from time to time. The more in tune we become with our biometric data, our behavior harmonizes along.
There is minimal risk in under training whereas risk in over training can be alleviated using wearable devices to assess recovery and promote best decision making. Individual athletes are not the only ones harnessing the insights of biometric data. Biometrics are making their way into the professional setting; employing biometrics as a team, steps competitions, and carefully choosing the fellow to lead an important meeting based on biometric data. Hospital systems are using biometric data and recovery scores to analyze anesthesiologists, surgeons, and nurses during surgery (Meltzer, 2020). RPM extends even further to train conductors and bus drivers, where biometric analysis and workplace safety are being studied.
Even though most people can’t get to 10,000 steps, gamifying the experience of walking is inspiring people to monitor and act on their health. Research shows a positive correlation between health and productivity. Access to wearable technology and RPM is upping the standards for everyone’s health. Biostrap’s RPM software allows for up to 5 people tracking, making for great family engagement.Group analysis poses risks of score discrimination by inappropriate interpretation. biometrics as a team has a phenomenal future ahead because as a family, we are here to help you, you are a part of the family, and we want you to be taken care of.
Day to day decision making will adjust as consistency, regularity, and how much sleep we need change. Timing meals and exercise using biometric data reference will have you jumping out of bed feeling optimized. 2022 is a big breakthrough year in health care as the perspective begins to shift towards prevention-intervention and away from treatment-cure. Health is a journey throughout the lifespan. As our cells age microscopically, so do we physically. Wearable technology makes the invisible, visible by quantifying biometric data for health optimization.
References
Bryson, A., Arthur, R., & Easton, C. (2021). Prior Knowledge of the Grading Criteria Increases Functional Movement Screen Scores in Youth Soccer Players. Journal of strength and conditioning research, 35(3), 762–768. https://doi.org/10.1519/JSC.0000000000002724
Centi, A. J., Atif, M., Golas, S. B., Mohammadi, R., Kamarthi, S., Agboola, S., Kvedar, J. C., & Jethwani, K. (2019). Factors Influencing Exercise Engagement When Using Activity Trackers: Nonrandomized Pilot Study. JMIR mHealth and uHealth, 7(10), e11603. https://doi.org/10.2196/11603
Chapel, J. M., Ritchey, M. D., Zhang, D., & Wang, G. (2017). Prevalence and Medical Costs of Chronic Diseases Among Adult Medicaid Beneficiaries. American journal of preventive medicine, 53(6S2), S143–S154. https://doi.org/10.1016/j.amepre.2017.07.019
Colombetti E. (2014). Contemporary post-humanism: technological and human singularity. Cuadernos de bioetica : revista oficial de la Asociacion Espanola de Bioetica y Etica Medica, 25(85), 367–377.
Covid-19 map. Johns Hopkins Coronavirus Resource Center. (n.d.). Retrieved June 22, 2022, from https://coronavirus.jhu.edu/map.html
Hermida, R. C., Ayala, D. E., Mojón, A., Smolensky, M. H., Portaluppi, F., & Fernández, J. R. (2014). Sleep-time ambulatory blood pressure as a novel therapeutic target for cardiovascular risk reduction. Journal of human hypertension, 28(10), 567–574. https://doi.org/10.1038/jhh.2014.1
Kent, C. (2021, May 24). Wearables and Health Tracking: Photonics could reinvent the Apple Watch. Medical Device Network. https://www.medicaldevice-network.com/analysis/apple-watch-photonics/#:~:text=Apple%20was%20recently%20revealed%20to%20be%20a%20key,a%20special%20purpose%20acquisition%20company%20%28SPAC%29%20last%20month.
Meltzer, A. J., Hallbeck, M. S., Morrow, M. M., Lowndes, B. R., Davila, V. J., Stone, W. M., & Money, S. R. (2020). Measuring Ergonomic Risk in Operating Surgeons by Using Wearable Technology. JAMA surgery, 155(5), 444–446. https://doi.org/10.1001/jamasurg.2019.6384
Rudin, R. S., Fischer, S. H., Damberg, C. L., Shi, Y., Shekelle, P. G., Xenakis, L., Khodyakov, D., & Ridgely, M. S. (2020). Optimizing health IT to improve health system performance: A work in progress. Healthcare (Amsterdam, Netherlands), 8(4), 100483. https://doi.org/10.1016/j.hjdsi.2020.100483
Sabry, F., Eltaras, T., Labda, W., Alzoubi, K., & Malluhi, Q. (2022). Machine Learning for Healthcare Wearable Devices: The Big Picture. Journal of healthcare engineering, 2022, 4653923. https://doi.org/10.1155/2022/4653923
Telehealth policy trend maps. CCHP. (2021, April 15). Retrieved June 22, 2022, from https://www.cchpca.org/policy-trends/
Wong, C. K., Ho, D., Tam, A. R., Zhou, M., Lau, Y. M., Tang, M., Tong, R., Rajput, K. S., Chen, G., Chan, S. C., Siu, C. W., & Hung, I. (2020). Artificial intelligence mobile health platform for early detection of COVID-19 in quarantine subjects using a wearable biosensor: protocol for a randomised controlled trial. BMJ open, 10(7), e038555. https://doi.org/10.1136/bmjopen-2020-038555
Workforce Health And Productivity. (2017). Health affairs (Project Hope), 36(2), 200–201. https://doi.org/10.1377/hlthaff.2016.1580